September brings a whole host of other important recognitions/observances including the start of Hispanic Heritage Month, World Suicide Prevention Day (Sept. 10), Stand Up to Cancer Day (Sept. 12), World Alzheimer’s Day (Sept. 21). The root of the word courage is cor-, the Latin word for heart. Sept. 29 marks World Heart Day – a day to recognize that one in five people die early from cardiovascular disease while 80% of heart disease and stroke cases are preventable. Click this link to learn more about World Heart Day (About - World Heart Federation).
To keep it brief this month … two important topics:
1) Be sure to complete your annual Corporate Integrity Agreement Training in HealthStream. Providers who are incomplete on Sept. 15 will have their privileges administratively suspended … so get it done now! If you have questions about your status, please contact the Med Staff Office.
2) Length of Stay – on the decline but challenges remain. Our targets for 2025 are 5.3 days at Providence St. Peter Hospital and 4.17 days at Providence Centralia Hospital. Kudos to Providence Centralia for exceeding their target in August (reached 3.98 days!). For St. Peter, while we reached an all-time low of 5.55 days, we have hovered here for the past 4-5 months at around 5.5-5.6 days. This will be challenged by our upcoming respiratory season and potentially lower than typical vaccine uptake. I’d like to ask for your assistance in two areas here:
a. Getting to know GMLOS – the Geometric Mean Length of Stay (GMLOS) is used to estimate the expected length of an inpatient hospital stay. It’s important for three big reasons: it helps allow meaningful coordination of care (anticipating that most patients with a particular diagnosis will discharge after 4 or 5 days), helps determine when patients may be off track (if a patient with a DRG of Septicemia or Severe Sepsis without Mechanical Ventilation >96 hours without MCC has a GMLOS of 4.9 days, what are the reasons they remain inpatient at 9 days?) and it is a key component for CMS reimbursement (reimbursement is fixed per DRG). It’s a place to start discussions with the care team about how we get patients ready for their next site of care and NOT
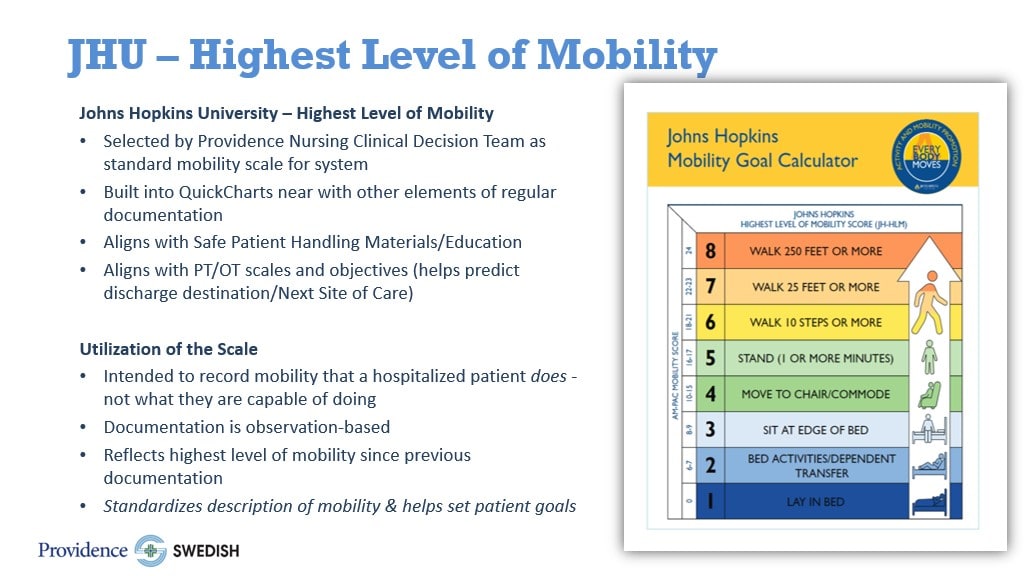
b. Mobility, mobility, mobility! Hospitalized older adults often spend more than 80% of their time in bed, leading to functional decline. Our nursing leaders are rolling out ways to get our patients up and moving! I need your help in ensuring that ALL patients 1. highest level of mobility score documented within 24 hours of admission (Johns Hopkins Highest Level of Mobility (JH-HLM, see scale and additional info below)) by nursing and 2. have mobility orders based on your recommendation for activity.