
Dr. Omid Mehdizadeh explains how Inspire, a minimally invasive therapy for treating obstructive sleep apnea, works.
For people with obstructive sleep apnea (OSA), a common condition in which the person's airway fully or partially closes while they're sleeping, waking up gasping for breath is the least of their problems. Even moderate OSA is implicated in a host of serious health issues, including cardiovascular disease, dementia, depression and diabetes. That’s why treating it is so critical, says Omid Mehdizadeh, M.D., an otolaryngology and head and neck surgeon at the Pacific Neuroscience Institute at Providence Saint John’s Health Center.
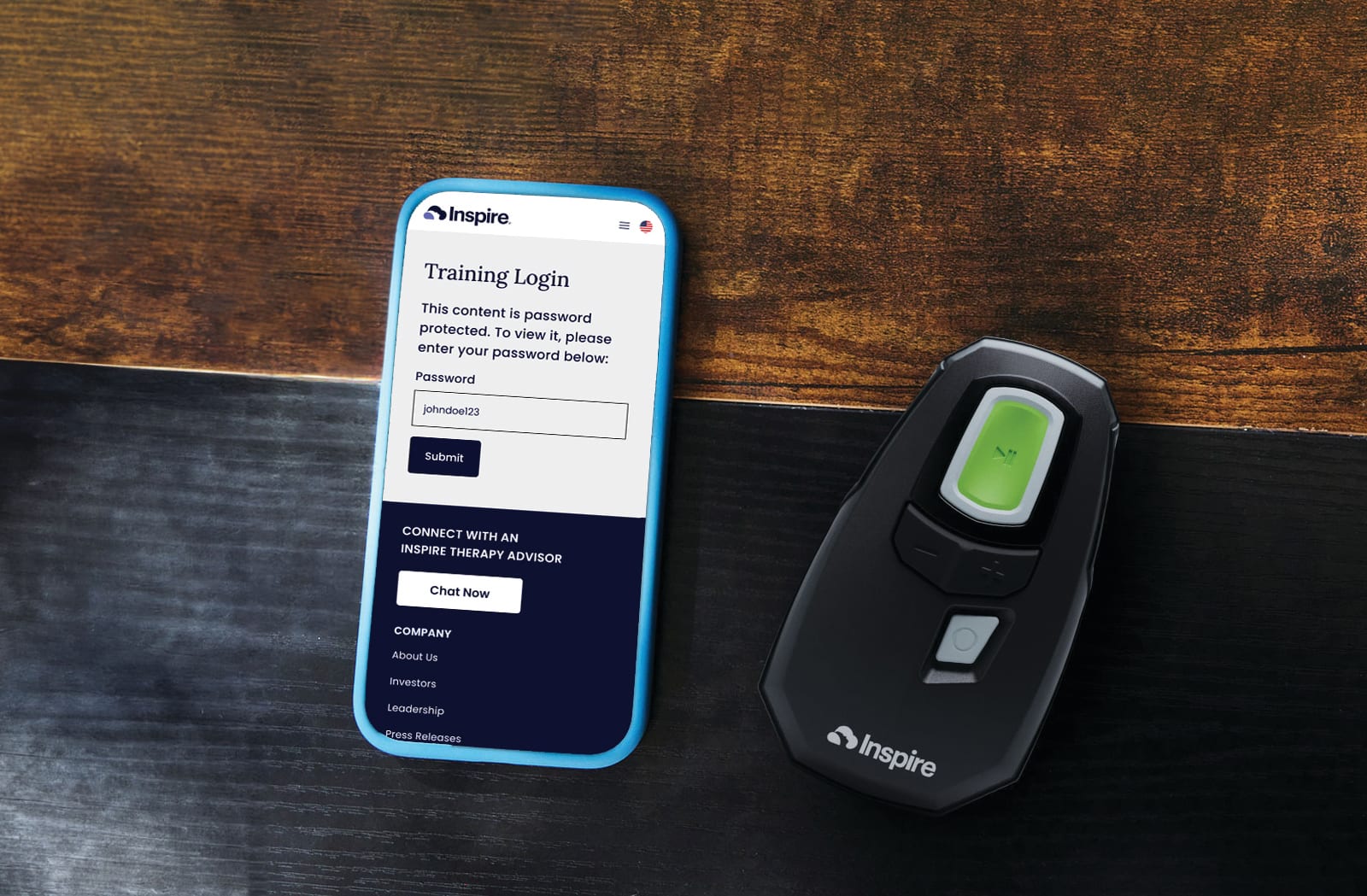
While the conventional therapy for OSA is continuous positive airway pressure (CPAP), which connects patients to a machine that delivers pressurized air via a mask and hose during sleep, many find the system uncomfortable and inconvenient. More recently, a mask-free option became available: Inspire therapy, an app-controlled unit that’s implanted in the chest wall and keeps the airway open by stimulating the throat muscles with electrical pulses. Here, Dr. Mehdizadeh talks about the advance that Inspire represents in OSA treatment and what other options there are for OSA.
Is anyone with sleep apnea a candidate for Inspire?
The Inspire system is mainly for obstructive sleep apnea. There’s central apnea and mixed apnea, which have to do with the brain not sending signals to the body to breathe. Inspire is generally not indicated for that. Central and mixed events have to be less than a quarter of total obstructive events for the person to qualify.
If I’m newly diagnosed with obstructive sleep apnea, can I go straight to getting an Inspire unit?
No, you have to have tried CPAP and failed it first. CPAP is still considered the gold standard of treatment: It’s the lowest-risk treatment for moderate to severe sleep apnea. We determine the severity of your OSA with the apnea-hypopnea index (AHI), and that score needs to be less than 100 for Inspire. Patients need to have a body mass index (BMI) of less than 40, although some insurance asks for a BMI of less than 35. And prospective patients need to undergo a procedure called a drug-induced sleep endoscopy.
How long is the Inspire implant procedure?
The procedure takes an hour and a half to two hours, and it’s an outpatient surgery done under general anesthesia. What’s unique about Inspire is that it can treat very difficult sleep apnea while not being as invasive as other sleep apnea surgeries.
What are the other surgical options like?
It all depends on the patient’s anatomy. Options range from throat surgery, including soft palate surgery, to tonsil or tongue surgery. We may involve nasal surgery, because improving nasal breathing reduces the number of events of apnea as well. On occasion, we need to do voice box surgery if it’s the voice box that’s collapsing into itself. And then there’s jaw surgery for severe sleep apnea called maxillomandibular advancement, which is essentially cutting the jawbone and the midface bone and moving them forward to open up the airway.
That sounds really complex.
Yes. In that surgery, you are changing the appearance of the face, because you’re moving the midface and the lower face — the jaw — forward.
Is it possible to have sleep apnea and not know it?
Yes. I would say that we hear that pretty often from patients—that they’re not aware of any symptoms at all.
But if you don’t suspect you have OSA, how would you get diagnosed?

Most of the time it’s the patient’s partner noticing something. They’re seeing their partner choking in their sleep or there’s severe snoring. Then, when I ask the patient questions, I see that there’s a pattern. Or it may be a referral from another doctor. For example, their cardiologist will see an abnormal heart rhythm and refer them for a sleep study.
How long does it take to get Inspire working?
From the time the patient first sees the surgeon to activation is four to six months. Once I determine they’re a candidate, I schedule surgery to implant the Inspire device. I see them in a post-op visit, just ensuring everything is OK. Six weeks after surgery, Inspire is turned on for the first time. The patient is taught how to use it. They’re shown how to increase the amplitude of the stimulation every week. About three months after surgery, they repeat their sleep study to assess their response to the surgery. It’s a collaboration between the surgeon and the sleep medicine physician.
Are there any limitations imposed by the device?
After the postoperative recovery period, there are absolutely no restrictions. It doesn’t go off in a metal detector. You’re allowed to get MRIs.
To schedule a consultation with Dr. Mehdizadeh, call 310-829-8701 (Santa Monica) or 310-477-5558 (Los Angeles).
Could You Have Sleep Apnea?
With more than three million cases of sleep apnea diagnosed each year, the condition is seen in all age groups. However, you're more likely to develop it as you grow older. Obstructive sleep apnea is more common in men than in women, although risk for women rises after menopause.
Other risk factors include:
- Endocrine disorders, including low thyroid hormone levels
- Excess weight
- Family history of OSA
- Jaw misalignment
- Large neck circumference
- Large tonsils
- Narrow airway
- Smoking
- Use of sedatives, including alcohol, opioid medications and tranquilizers
If you suspect you might have OSA, watch for symptoms that may include loud snoring, waking up gasping or choking, morning headaches or dry mouth, and extreme daytime sleepiness. See your primary care physician or sleep specialist for an evaluation.



















