By Dr. Alexander Katz
SOUTH PUGET SOUND — Medication reconciliation at admission is a core attending physician’s responsibility and a critical patient-safety function. National data consistently demonstrates medication discrepancy rates exceeding 50% during transitions of care. With limited pharmacy resources available for real-time reconciliation, provider vigilance is essential.
One method to verify the most recently dispensed outpatient medications is to review pharmacy fill history via Surescripts in Epic.
Use Surescripts in Epic (medication dispense history)
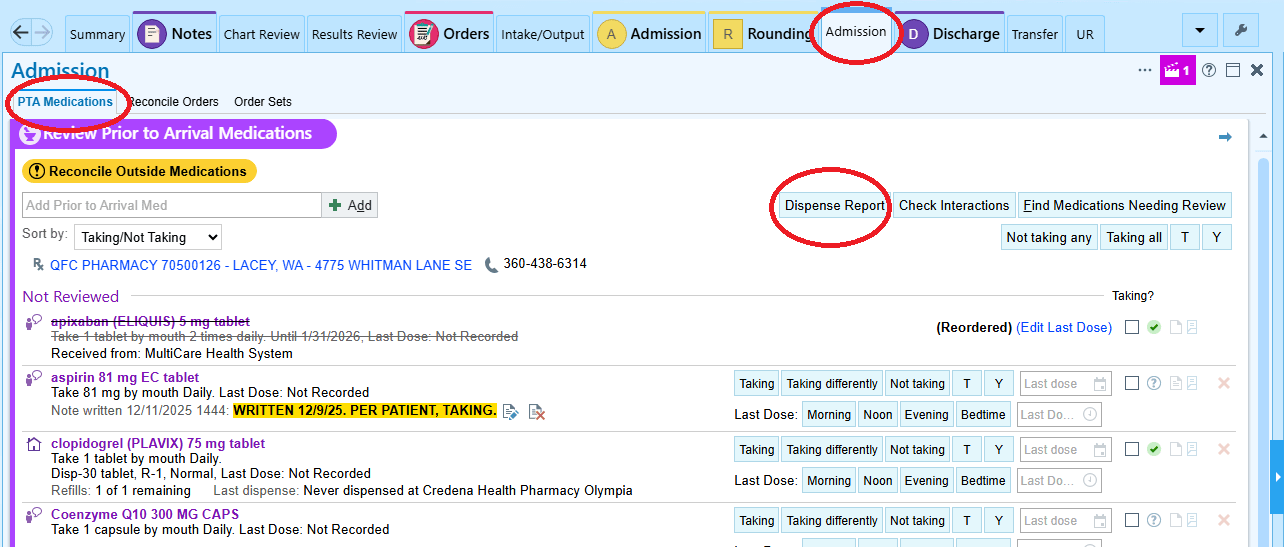
Access via Admission → PTA Medications → Dispense Report.
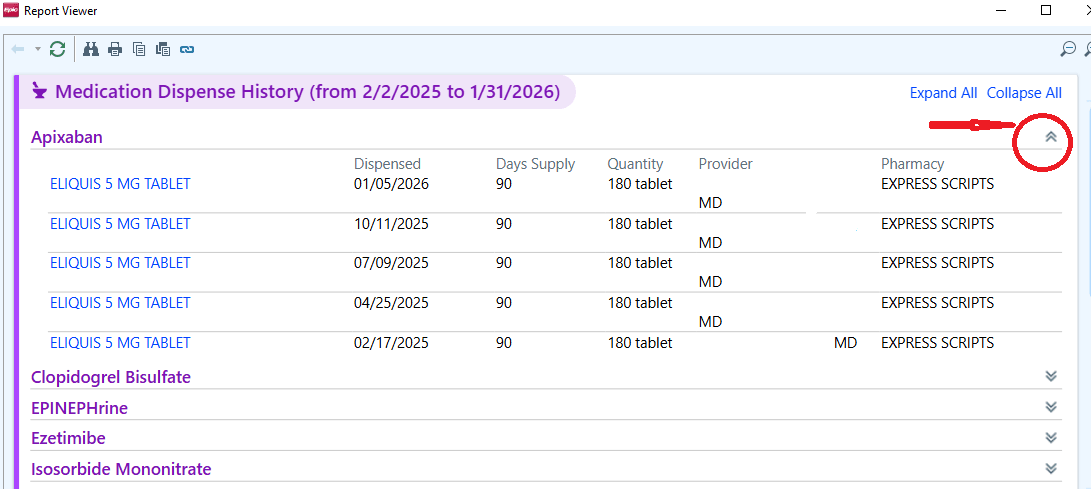
- Expand the medication of interest to review dispense dates, days supply, quantity and pharmacy source.
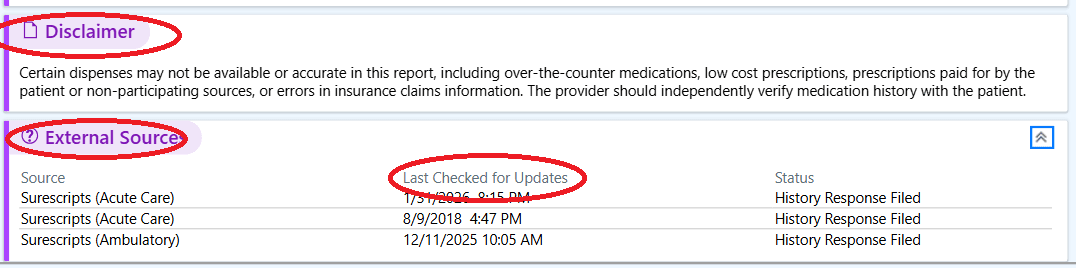
- Always review the disclaimer and the “Last Checked for Updates” timestamp.
Additional high-yield checks
- Check Care Everywhere for recent admissions, Emergency Department visits and medication changes.
- For patients arriving from facilities (SNF, LTACH, rehab), obtain a MAR or facility medication list rather than relying on patient recall.
- Clarify who manages the patient’s medications (patient, caregiver or facility), particularly in elderly or cognitively impaired patients.
Prioritize high-risk medications
- Anticoagulants
- Insulin / hypoglycemics
- Antiepileptics
- Cardiac medications
- Opioids / sedatives
- Immunosuppressants
Professional society & safety resources
Agency for Healthcare Research and Quality (AHRQ) – Medication Reconciliation Primer
AHRQ’s Patient Safety Network (PSNet) defines medication reconciliation as a structured process done during hospital admission, transfer, and discharge, comparing a patient’s medication history with new orders to identify discrepancies.
Accurate medication reconciliation at admission is one of the most impactful actions to prevent avoidable harm. By consistently using available tools such as Surescripts, verifying information across care settings and prioritizing high-risk medications, providers can markedly reduce discrepancies during this transition of care. Thoughtful, methodical reconciliation — especially when pharmacy support is limited — reinforces patient safety, supports continuity of treatment, and sets the foundation for safer inpatient and discharge medication management.













